Drilling, Fixation And Osteochrondral Grafts
Home » Operations » Knee Surgery » Osteochondritis Dissecans Surgery » Drilling, Fixation And Osteochrondral Grafts
What is the problem?
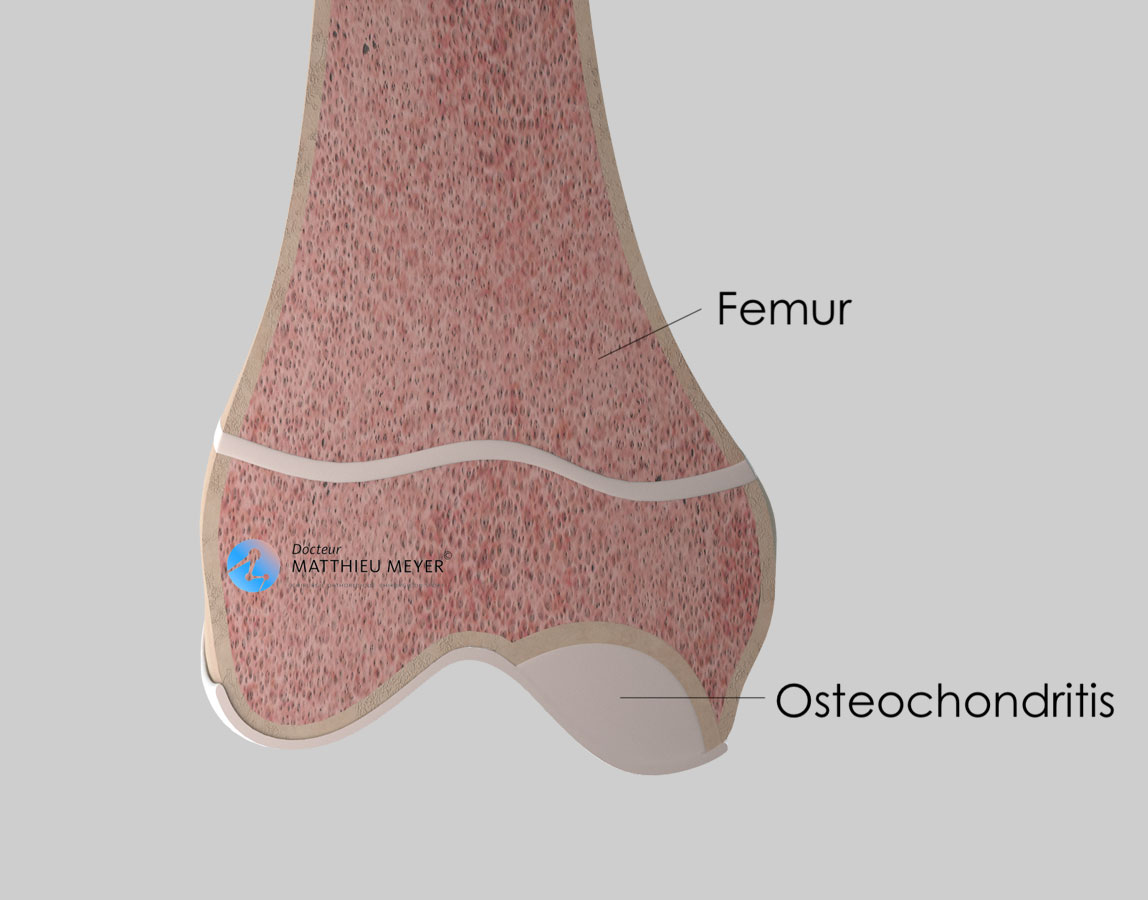
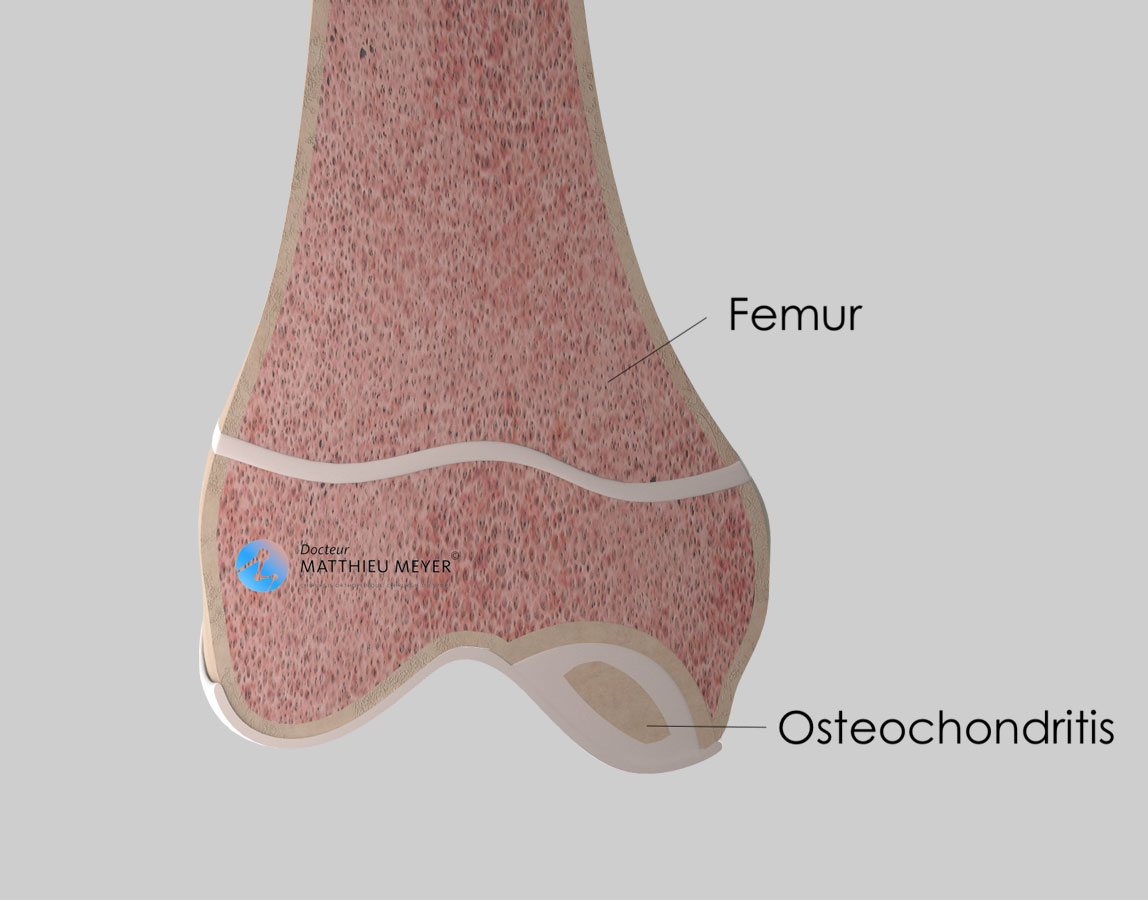
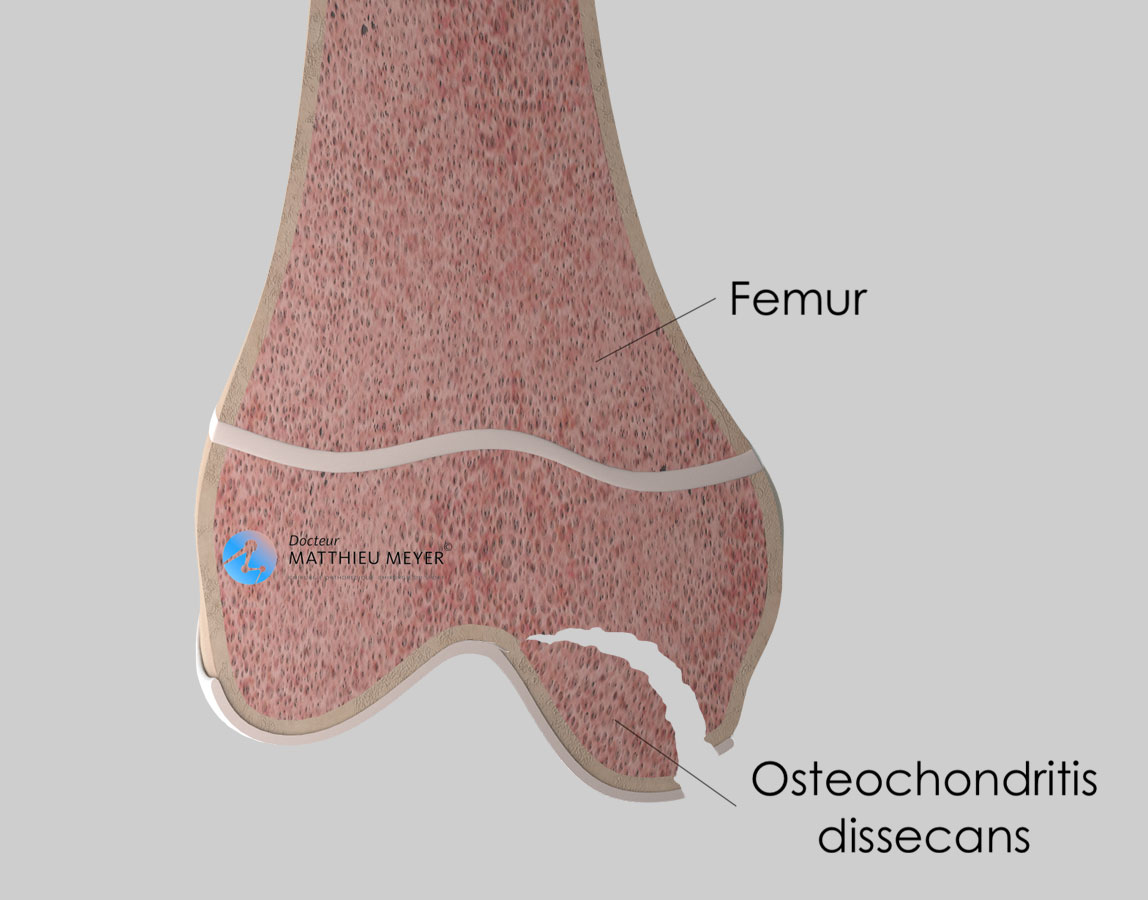
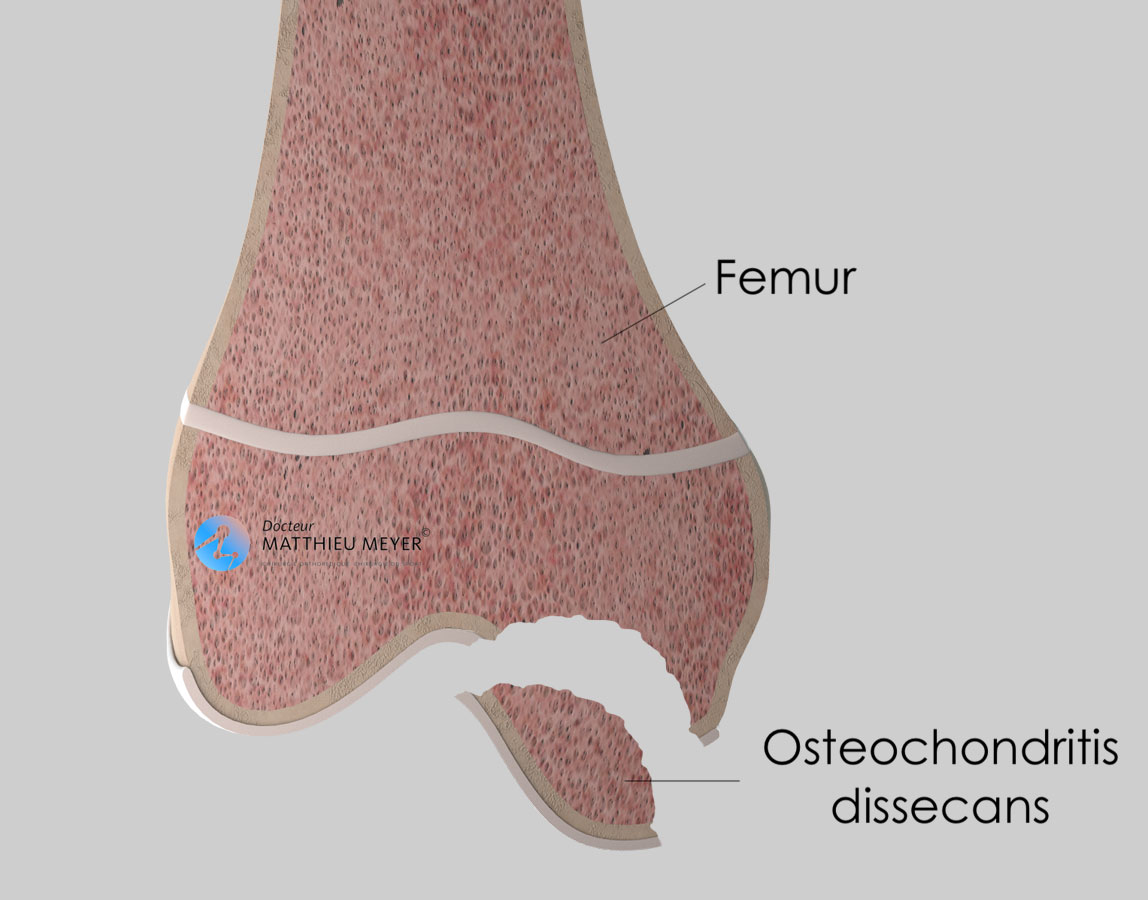
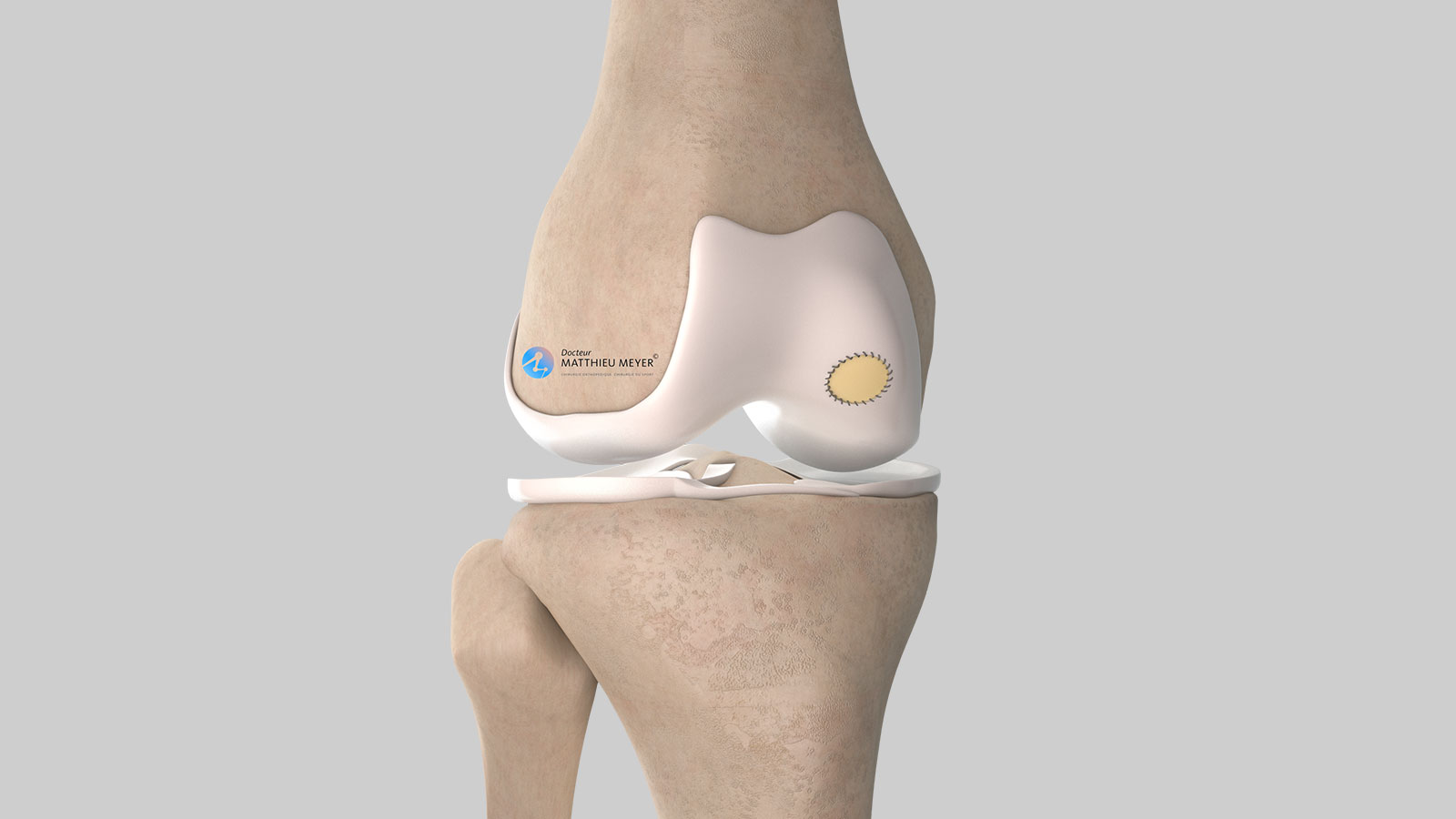
Osteochondritis dissecans is the localized deterioration of the bone directly under the cartilage, near the joint. It can result in the detachment of a fragment of bone and adjacent joint cartilage called an osteochondral fragment and the onset of knee osteoarthritis.
Its cause is not clearly established but repetitive microtrauma resulting from some anatomical configurations could probably explain its onset.
Osteochondritis is relatively rare, affecting 0.1% of the population and predominantly young male athletes. The initial symptoms often develop between the age of 10 and 20 years. In the knee, osteochondritis predominantly affects the medial femoral condyle.
Natural progression of osteochondritis dissecans
Complete radiological and clinical healing is possible and prevalent when osteochondritis develops before the age of 12 years.
Beyond this age, it will probably worsen. However, osteochondritis can remain asymptomatic or just cause pain during exertion for several years.
The turning point in the progression of osteochondritis is when an osteochondral fragment comes loose in the joint, sometimes indicative of the pathology and causing pain and locking of the knee. At this stage, and in the absence of specialist treatment, cartilage wear (osteoarthritis) is inevitable.
The different stages of osteochondritis
It is important to identify the stage of the lesion to determine the most appropriate treatment. The most common method used is Bédouelle’s classification, which comprises 4 stages corresponding to the progression of osteochondritis.
What examinations are necessary?
X-rays are systematically used to diagnose osteochondritis, sometimes accidentally when the examination was prescribed for another reason.
An MRI will probably be conducted as well to determine if the cartilage is cracked and if the osteochondral fragment is loose, essential criteria when choosing the treatment. The injection of a contrast medium is sometimes required during the MRI to assess the vitality of the osteochondritis fragment, as this is sometimes taken into consideration when choosing the treatment.
Sometimes, an CT arthrogram (scan with the injection of a contrast medium in the knee) is preferred to an MRI and provides information comparable to that of an MRI but is sometimes more accurate regarding the condition of the cartilage.
Treatments available
Orthopaedic treatment
This non-surgical treatment is based on stopping high-impact or pivoting sports activities for 3 to 6 months and is for children or young adolescents whose skeleton is not fully developed. Immobilisation is unnecessary. This treatment is considered effective if the pain disappears after stopping sport for a maximum period of 6 months. Otherwise, surgical treatment must be considered.
Trans-chondral drilling
This surgical treatment is carried out using arthroscopic or video surgery through 2 incisions in the knee 5 millimetres in length. Small holes are drilled through the cartilage to the healthy area of the femoral bone in the area affected by osteochondritis. The aim is to cause bleeding and thus improve blood flow to the affected area of bone and encourage healing with the healthy femur.
This treatment is only effective if the skeleton is still growing for which the outcome is very good. If it is carried out once the skeleton is fully developed, the results are disappointing.
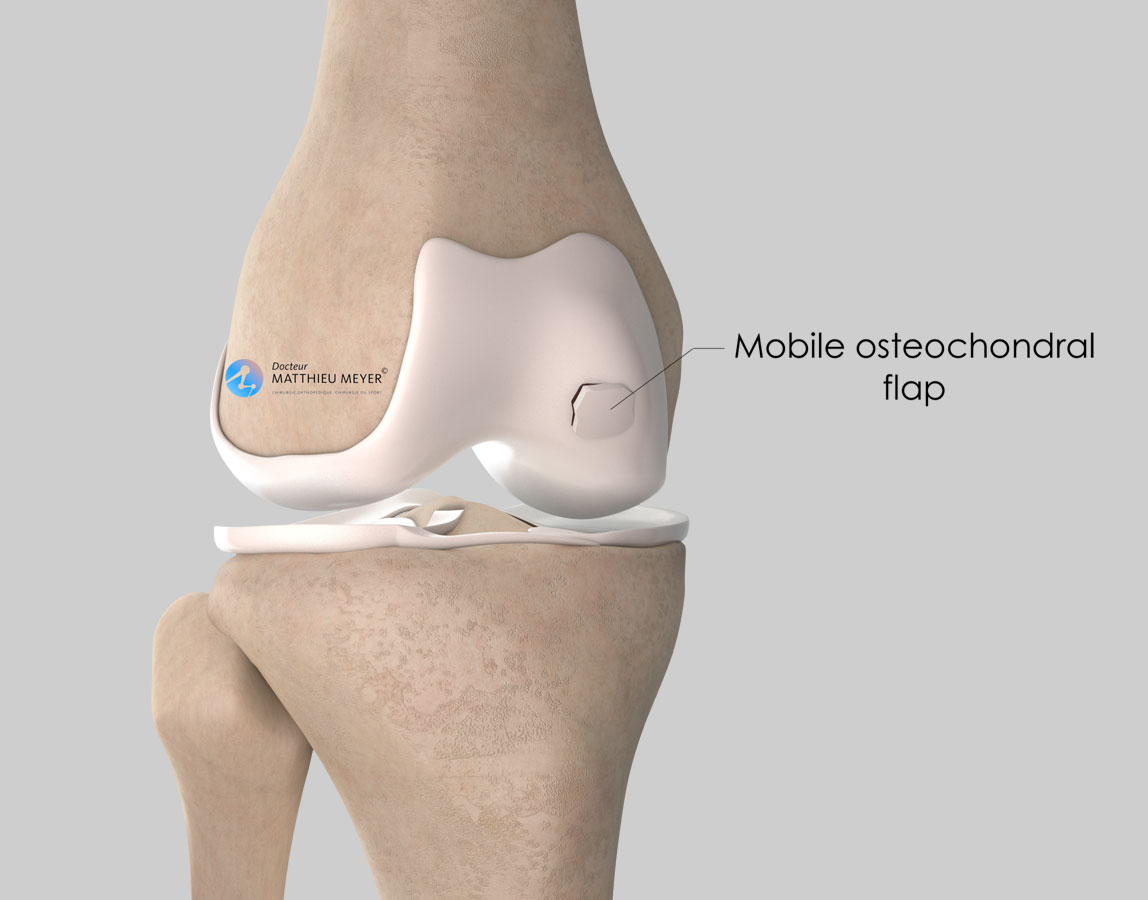
Fixation of a mobile osteochondral fragment
This treatment is indicated if the osteochondral fragment is mobile or even totally loose in the joint. However, the osteochondral fragment must be intact.
The mobile fragment can be fixed using one or several specific screws, one or several osteochondral autograft plugs or both according to the age of the patient, the vitality of the fragment, and the size of the lesion. Lesions deeper than 7 mm can also be filled with a cancellous bone autograft harvested from the tibia or the pelvis of the patient.
This treatment is generally carried out through a short incision in the joint (approximately 5 cm) or, in some cases, arthroscopically. When screws are used, they are buried deep in the cartilage and are not systematically removed.
Osteochondral reconstruction techniques
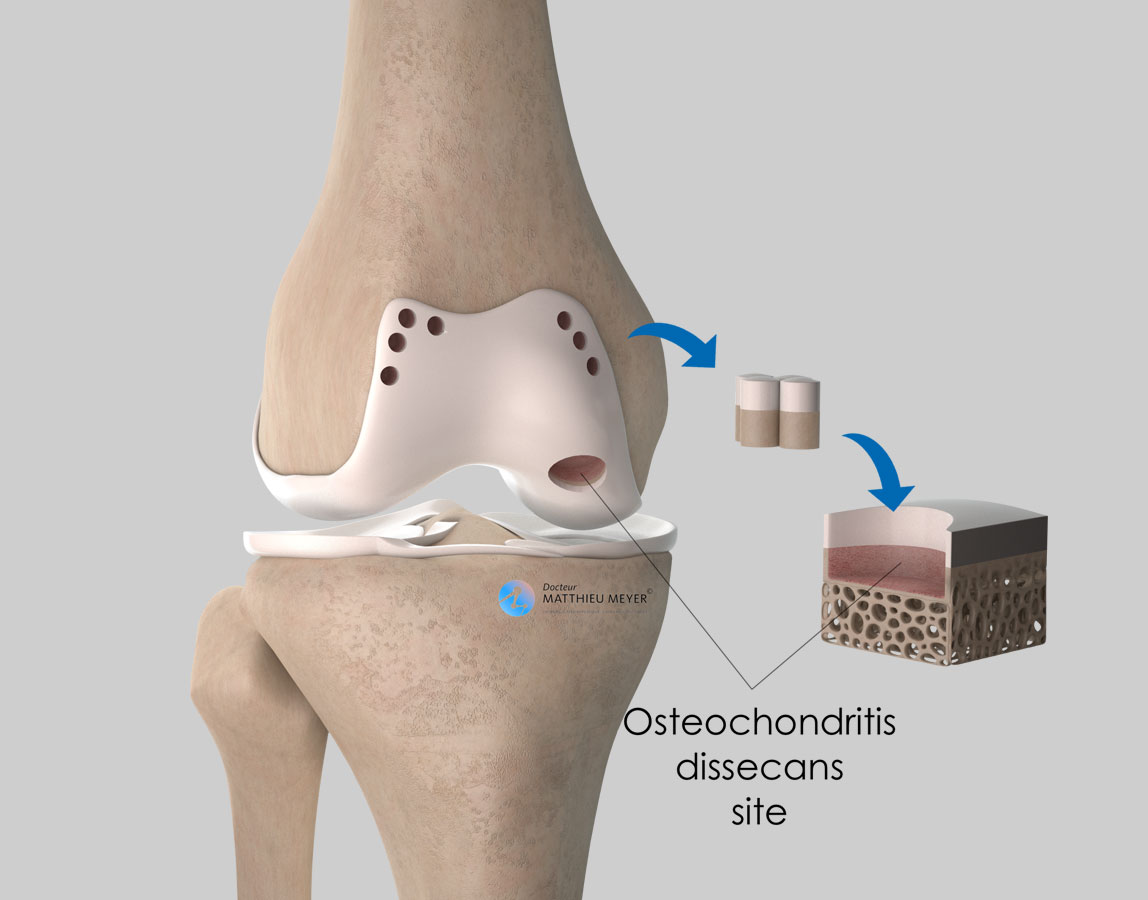
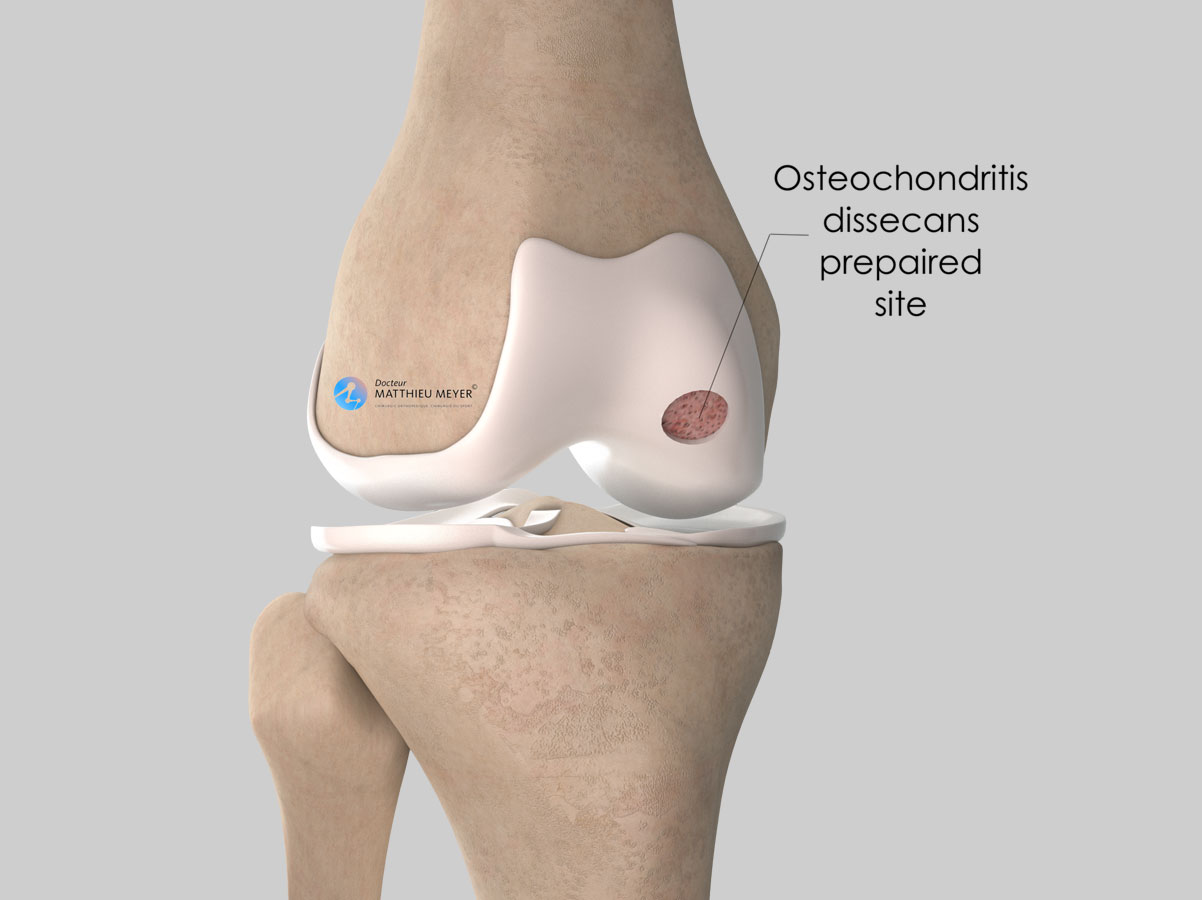
When the osteochondral fragment is too damaged to be reattached, its removal leaves an osteochondral defect (hole in the cartilage and underlying bone). There are various techniques available to fill this defect.
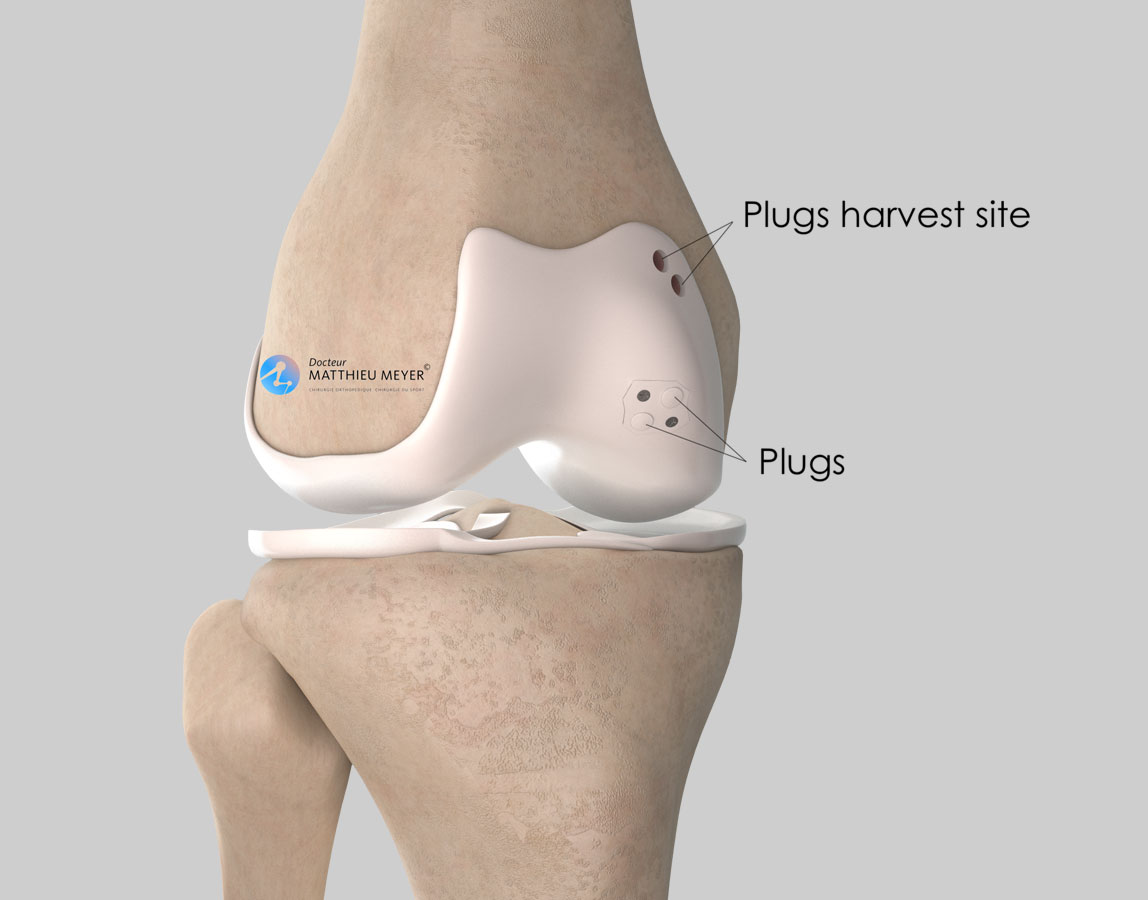
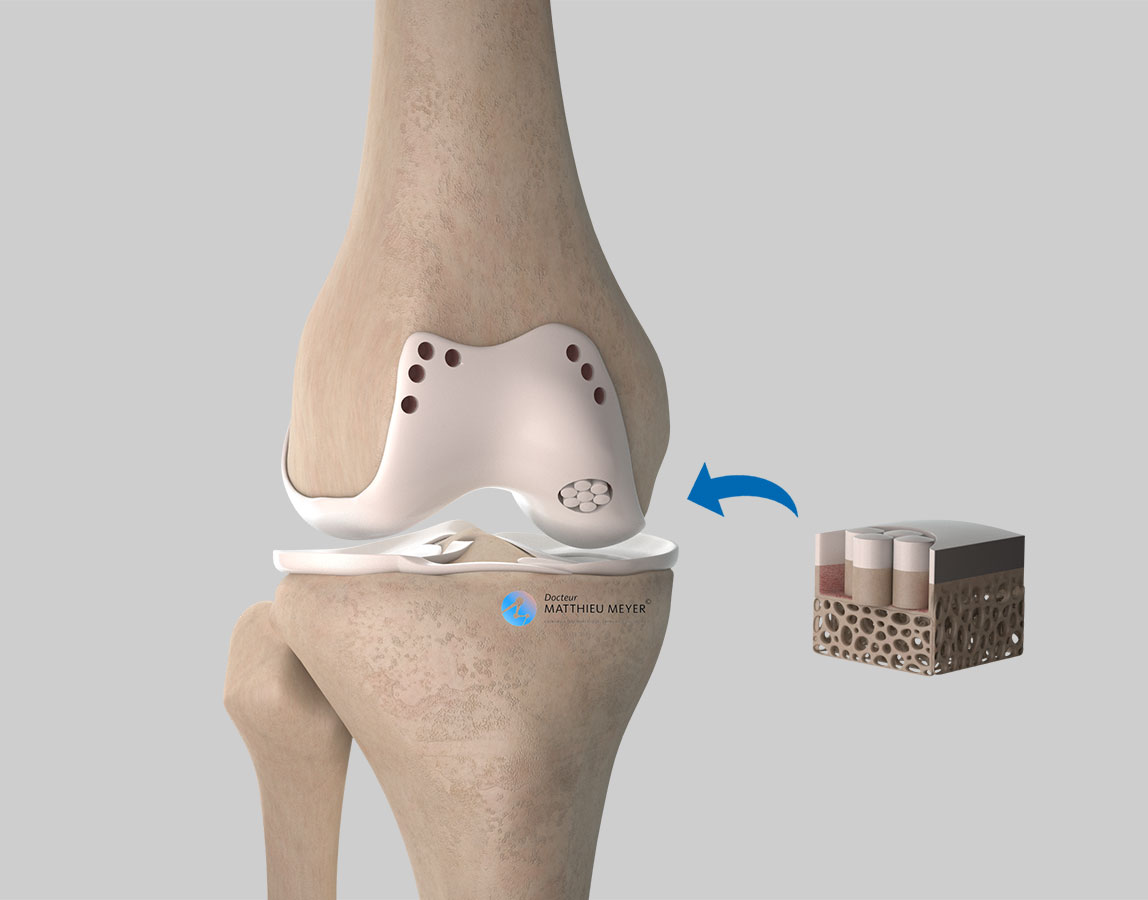
Osteochondral autograft (mosaicplasty)
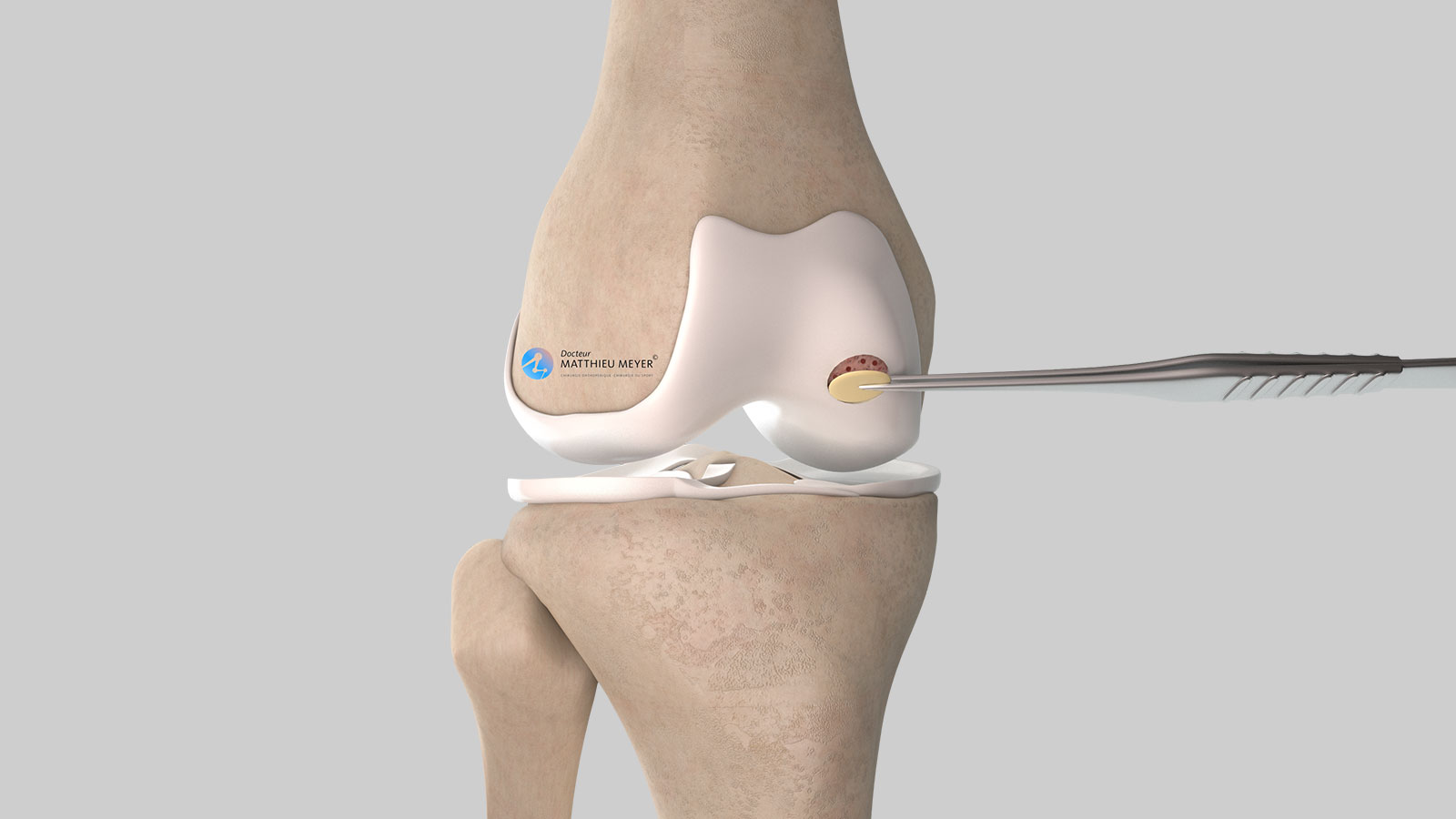
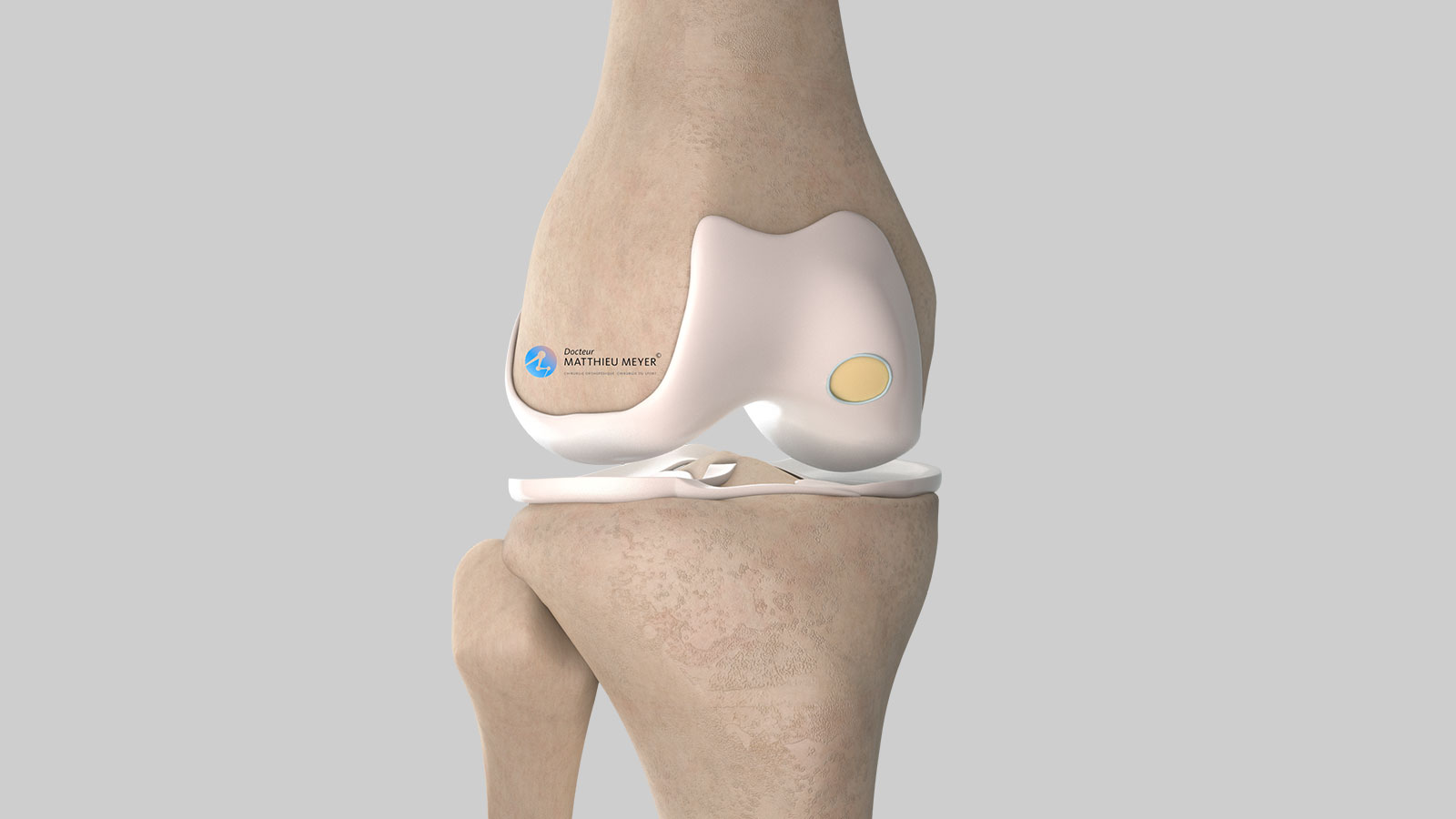
This technique consists in harvesting one or several osteochondral plugs (bone carrots topped with cartilage) that are transplanted into the defect. These plugs are harvested from parts of the knee where morbidity is low, that is lower weight-bearing areas.
As the area in the knee from which osteochondral plugs can be harvested is limited, this technique is only used for defects less than 4 cm2.
A mosaicplasty is generally carried out through a short incision in the joint (approximately 5 cm) or, for some small lesions, using arthroscopy. This effective, tried and tested technique produces lasting results but can sometimes leave some residual pain around the harvest site of the osteochondral plugs.
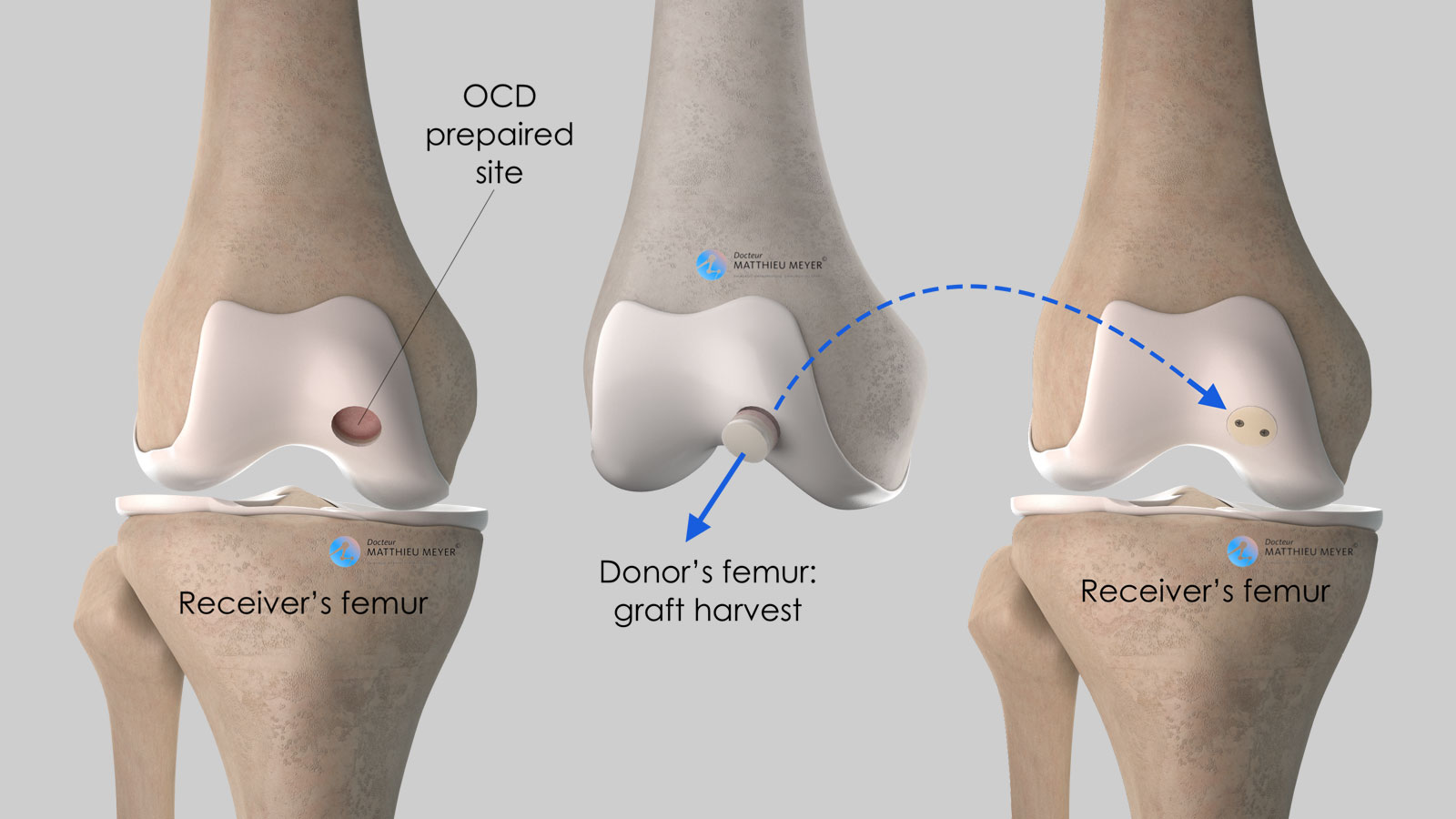
Osteochondral allograft
This technique is comparable to a mosaicplasty but unlike the latter, the plugs are harvested from the femur of a deceased donor, obtained within the framework of organ donation.
An osteochondral allograft is a “salvage” treatment indicated in the case of a large defect (> 4 cm2) that is generally filled with a single, large-diameter plug.
The results are good after 10 years with 90% of patients not requiring another operation.
This technique has the advantage of not causing any pain around the harvest site but is hampered by the low availability of grafts.
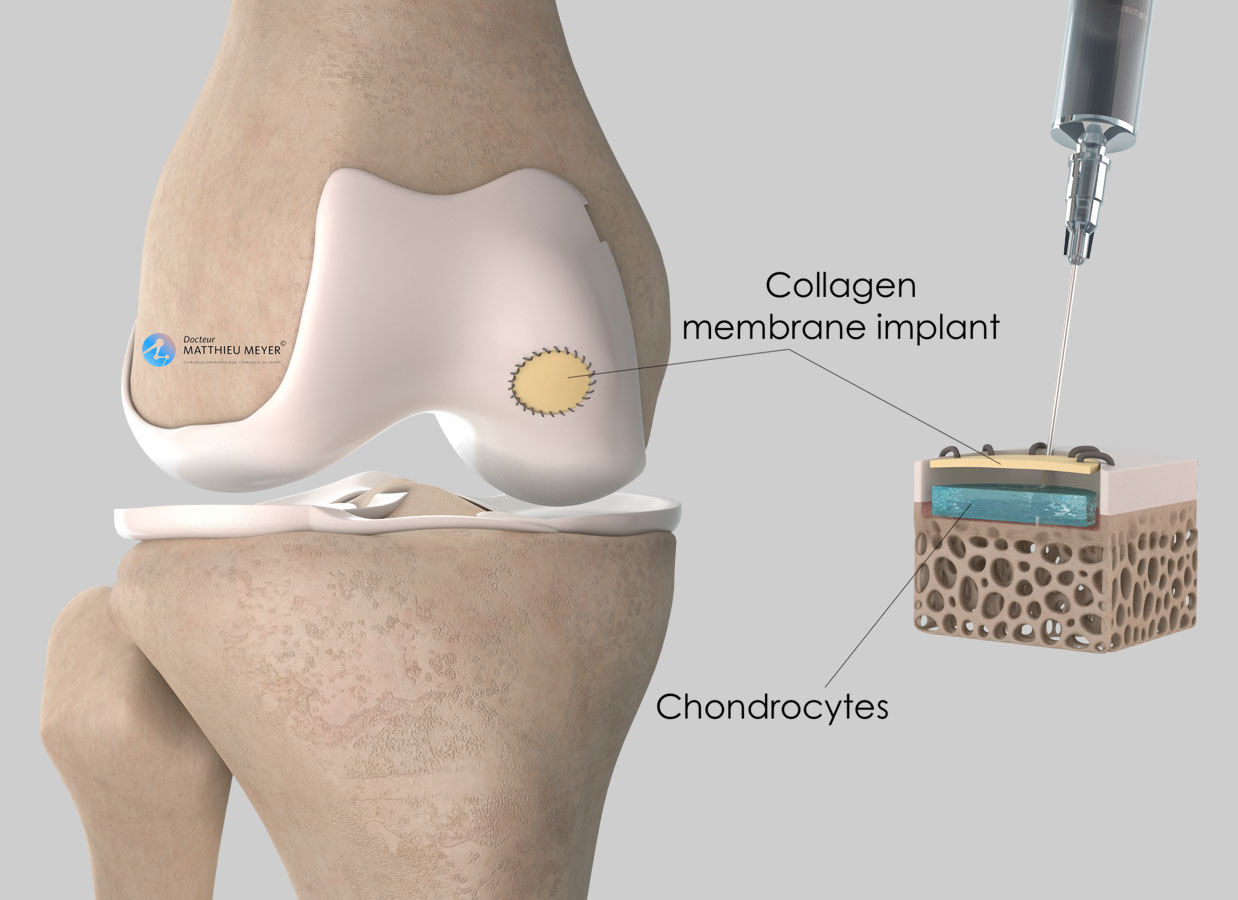
Microfractures, collagen membrane, cancellous autograft
The Microfracture technique consists in creating multiple holes in the exposed bone after removal of the osteochondral fragment. The aim is to cause bleeding bringing stem cells to the damaged area, which will help the lesion heal with the formation of fibrous cartilage tissue. However, the quality of the latter is not as good as the original hyaline cartilage.
The microfractures are created arthroscopically. If a collagen membrane is used, a short incision in the joint is necessary (approximately 5 cm).
The results of combining microfractures with a collagen membrane are globally not as good as a mosaicplasty with small lesions (< 2 cm2). However, it is an option for larger defects for which there are few alternatives.
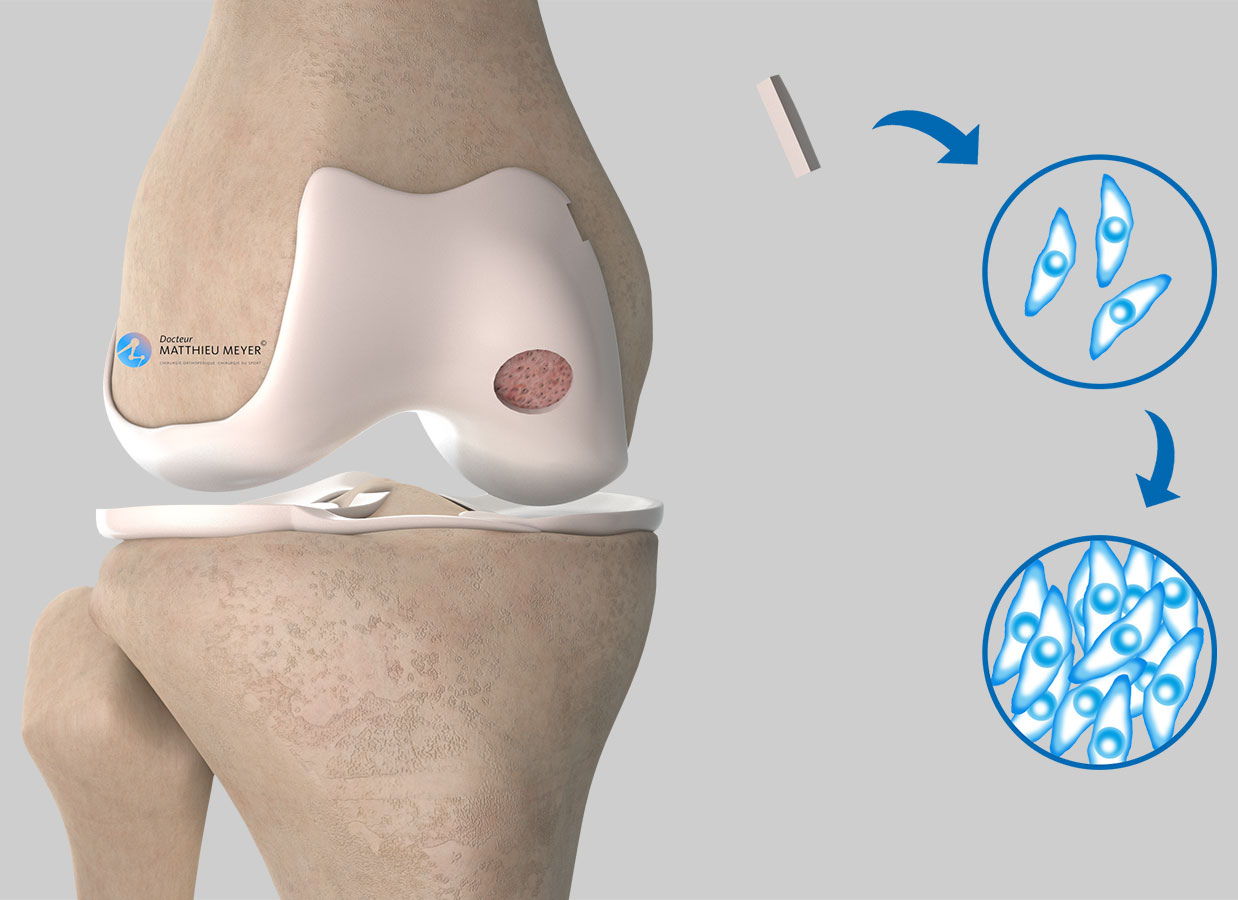
Autologous chondrocyte grafts
This technique is still being tested and assessed and cannot be used routinely as it requires authorisation and is reserved for certain hospital teams. This technique is carried out in 2 stages:
– 1st stage: Arthroscopic harvesting of a piece of healthy cartilage in the knee affected. This cartilage is then grown in a specialist laboratory to obtain a significant quantity of cartilage cells (chondrocytes)
– 2nd stage: 3 weeks later, through a short incision in the knee, a collagen membrane is placed over the defect. The defect may also be filled with a cancellous bone autograft harvested from the tibia or the pelvis. The cultivated chondrocytes are injected under the membrane and retained by the latter. Weight-bearing is resumed 6 weeks after the procedure.
The results of this technique are promising, particularly for large lesions but still need to be assessed.
Tibial or femoral osteotomy to realign the limb
Strictly speaking, this is not a method of treating osteochondritis dissecans but a surgical procedure that can be combined with the osteochondral fixation or reconstruction described previously.
Realignment is only considered if there is cartilage wear (osteoarthritis) around the osteochondritis lesion and if there is significant knee deformity (bowlegs or knock knee) likely to worsen the osteoarthritis damage.
In the case of bowlegs (genu varum), a high tibial osteotomy is carried out to realign the knee whereas in the case of knock knees (genu valgum) a distal femoral osteotomy is carried out to realign the knee.
Which treatment for which patients?
- In children and young adolescents still growing
Except in specific cases, stopping sport for 3 to 6 months is the first-line treatment. If the pain persists after this period, trans-chondral drilling will be proposed if the fragment is stable or fixation with screws or osteochondral plugs if it is mobile.
- In adults
In adults, the osteochondral fragment is often mobile and fixation is proposed if the condition allows. If this is not the case, a mosaicplasty will be performed if the lesion is quite small (< 4 cm2) or, for larger lesions, an osteochondral allograft or micro-fractures with a biological membrane (AMIC).
If there is osteoarthritis, a realignment osteotomy is sometimes combined.
Following all these surgical treatments, no weight-bearing is allowed on the operated limb for 6 weeks after the operation.
Mosaicplasty
Before the procedure
A mosaicplasty (or osteochondral autograft) requires an operation. Before the operation, a pre-anaesthesia consultation is conducted and possibly a pre-operative assessment to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications.
The procedure
The procedure takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed supine on an operating table and a tourniquet may be placed around the thigh but it is not always used. The operation lasts about 1 hour and can be carried out under general or spinal anaesthesia. The latter is a regional anaesthetic anaesthetising the lower part of the body (as with an epidural). The anaesthetist will decide on the most suitable anaesthetic together with the patient.
A mosaicplasty can be carried out arthroscopically or through a small incision of approximately 5 centimetres along the edge of the patella. The osteochondritis lesion is located then the remaining osteochondral fragments are removed and the defect flattened and reamed using a curette. Depending on the size of the lesion, one or several osteochondral plugs are harvested from areas around the edge of the femoral cartilage that are of less importance. Each plug harvested is then pushed into a hole drilled in the osteochondritis lesion (receiver site). At the end of the procedure, the osteochondritis lesion is filled with the osteochondral grafts. The holes left after harvesting the plugs will fill with fibrocartilage tissue within a few weeks.
At the end of the procedure, a drain is often inserted to prevent the formation of a haematoma.
After the procedure
After the procedure, the knee is partially numbed with a nerve block to help improve postoperative pain management. The effect lasts approximately 18 hours after the operation. Medication and ice on the knee also provide effective postoperative pain management.
After the operation, weight-bearing is not allowed on the leg operated on for 6 weeks and crutches must be used for walking. Weight-bearing can then be resumed. During this period, no brace is required and rehabilitation can begin early to mobilise the knee.
The stay in hospital generally varies from 1 to 2 days.
Check-ups are carried out at 6 weeks and 3 months to assess progress and detect any complications.
The duration of medical leave depends on the patient’s occupation but is often between 1½ and 3 months.
Driving can be resumed once weight-bearing is fully recovered. Low-impact non-pivoting sports can generally be resumed after 3 months and higher-impact sports after 6 months.
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics.
Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation.
Knee surgery and lack of weight-bearing on the limb operated on also increase the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed until weight-bearing is resumed, that is for 6 weeks after the operation.
In rare cases, the knee remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Finally, pain, often moderate, can remain around the site where the osteochondral plugs were harvested.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
In summary...
When is a mosaicplasty performed?
In the case of osteochondritis dissecans in adults if fixation of the osteochondral fragment is not possible
Aim of the operation
Relieve the pain and limit the risk of developing osteoarthritis
Which anaesthesia?
General or regional (determined with the anaesthetist)
Duration of hospitalisation
Between 1 and 2 days
Resumption of weight-bearing
6 weeks after the operation
After the operation
Return home
Duration of rehabilitation
Generally 2 to 3 months
Duration of medical leave
From 1½ to 3 months
Resumption of car driving
1½ months after the operation, when weight-bearing resumed
Resumption of sport
3 months after the operation for low-impact non-pivoting sports and 6 months for higher-impact sports
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib