Medial Opening-Wedge High Tibial osteotomy
Home » Operations » Knee Surgery » Surgery To Slow Knee Osteoarthritis » Medial Opening-Wedge High Tibial Osteotomy
What is the problem?
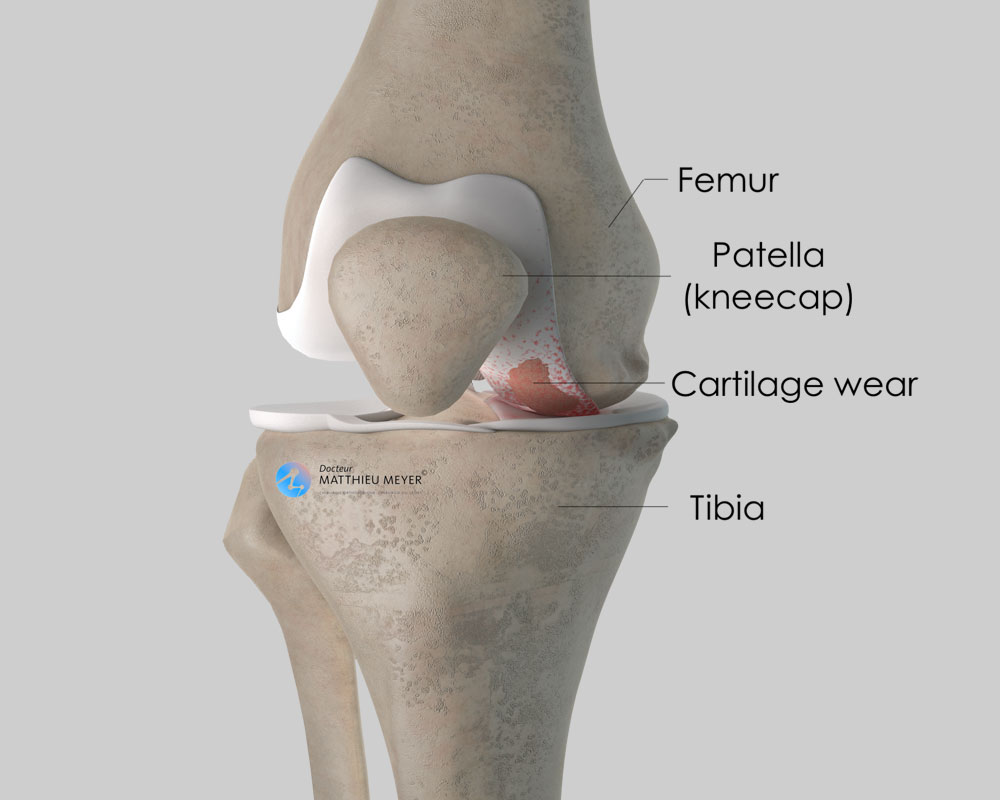
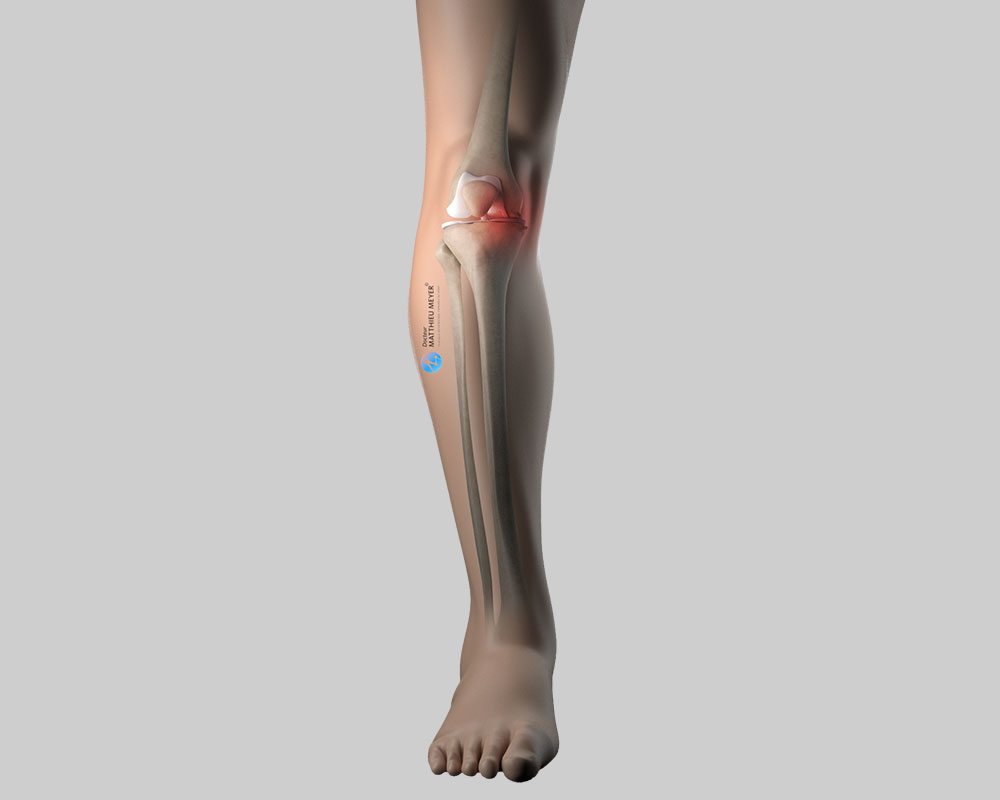
Like all joints, the knee is covered with cartilage, a slippery substance with no nerve endings that allows the joint to move freely and painlessly. This cartilage can wear for various reasons (excess weight, effects of ablation of a meniscus, consequences of a fracture…) exposing the underlying bone, which is rough and innervated; the joint gradually becomes stiff and painful. This is known as knee osteoarthritis or gonarthrosis.
When should a high tibial osteotomy be considered?
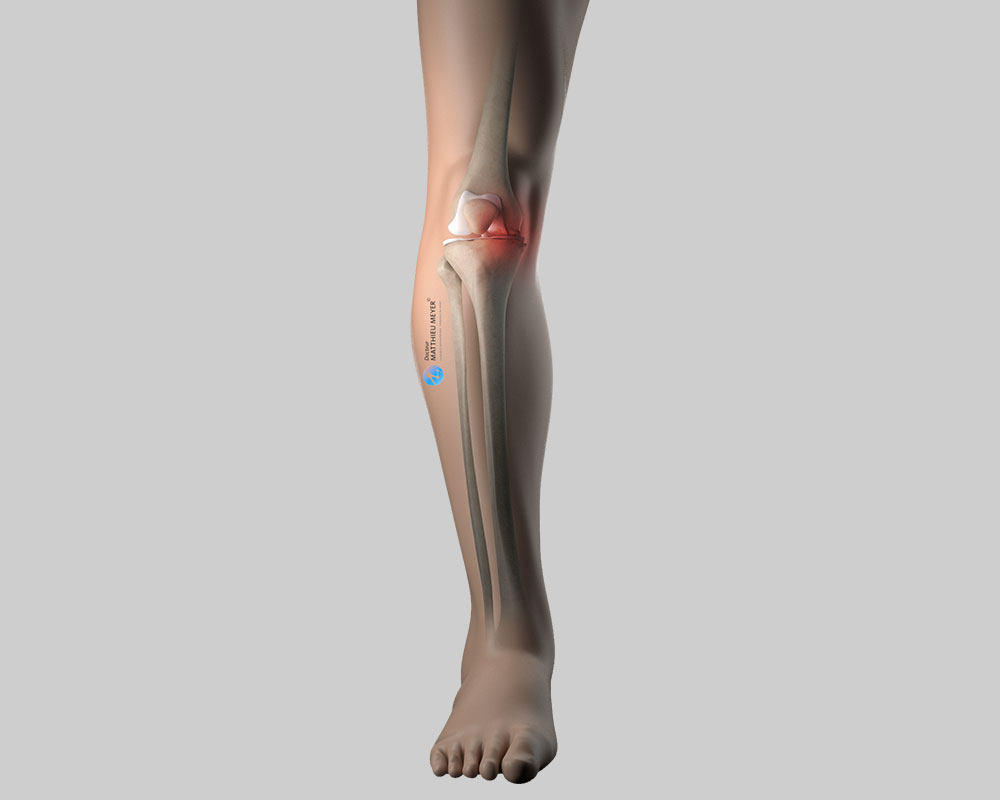
A high tibial osteotomy is indicated when only the medial femorotibial compartment of the knee is worn by osteoarthritis. A bowlegged (genu varum) deformity of the tibia can aggravate this osteoarthritis, as it increases the strain on the medial compartment of the knee and accelerates cartilage wear.
A high tibial osteotomy is only indicated when the cartilage in the medial part of the knee is not completely worn in patients under 60 who are considered too young to undergo a knee replacement.
This procedure consists in straightening the deformity of the tibia to transfer the mechanical load to the lateral part of the knee where the cartilage is not worn thus relieving the pain in the medial part of the knee, slowing the progression of osteoarthritis, and ultimately delaying a knee replacement.
This procedure is sometimes proposed in the absence of significant pain in relatively young patients with severe medial osteoarthritis. The problem with this type of osteoarthritis is the risk of it becoming painful once the cartilage wear is too severe and a high tibial osteotomy is no longer possible. This procedure may, therefore, be proposed in young patients to slow the progression of the osteoarthritis and avoid a knee replacement, even in the absence of pain.
Before the operation
A high tibial osteotomy requires an operation. The realignment necessary is determined during a scheduled consultation based on x-rays of all the lower limbs (hip-knee-ankle x-ray or EOS scan).
Before the operation, a pre-anaesthesia consultation is conducted to check the patient is physically apt to undergo the operation and minimise the risk of postoperative complications.
The operation
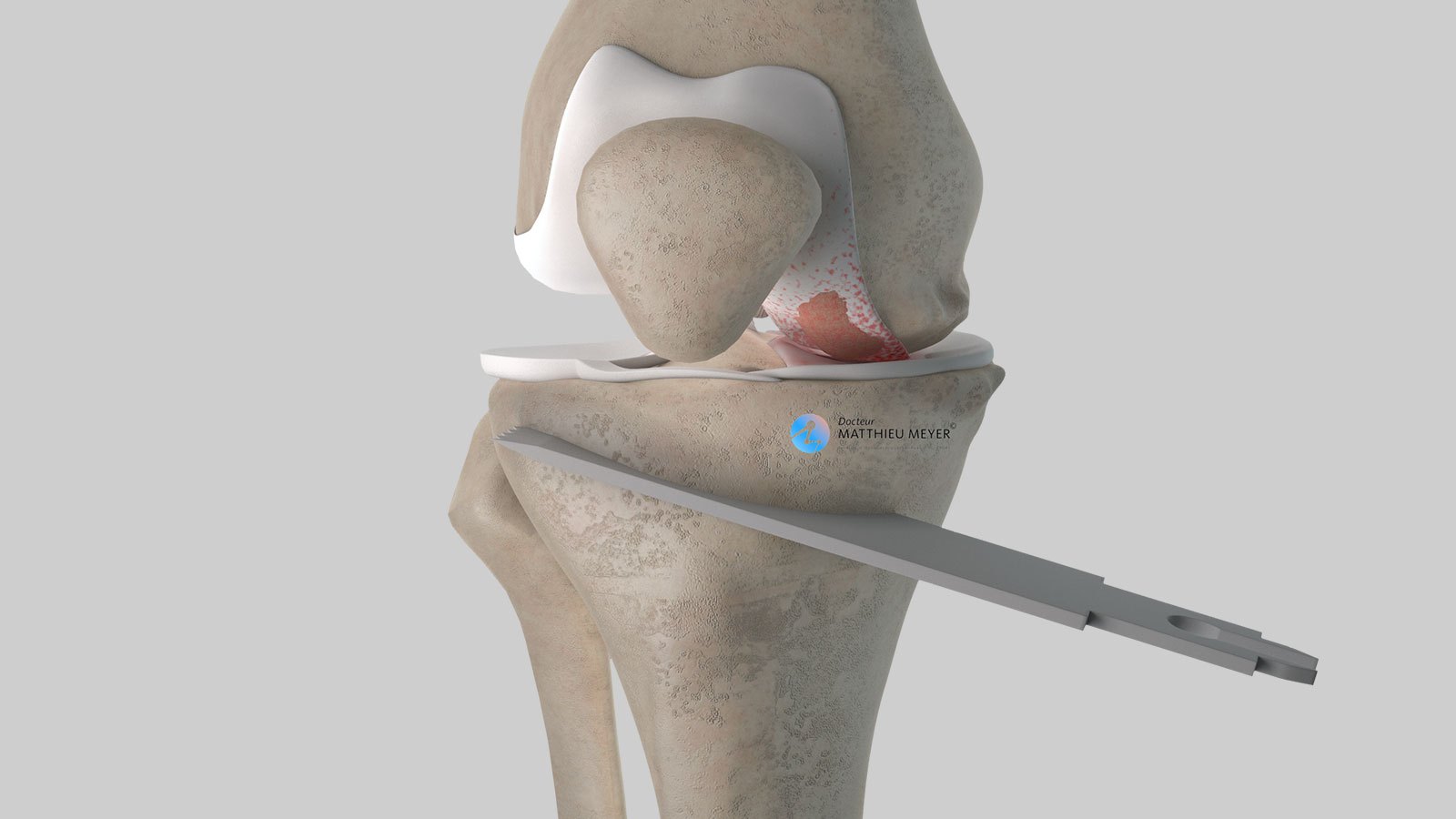
The operation takes place in an operating theatre in compliance with strict standards of cleanliness and safety. The patient is placed supine on an operating table and a tourniquet is placed around the thigh. The operation lasts about 1 hour and can be carried out under general or spinal anaesthesia. The latter is a regional anaesthetic anaesthetising the lower part of the body (as with an epidural). The anaesthetist will decide on the most suitable anaesthetic together with the patient.
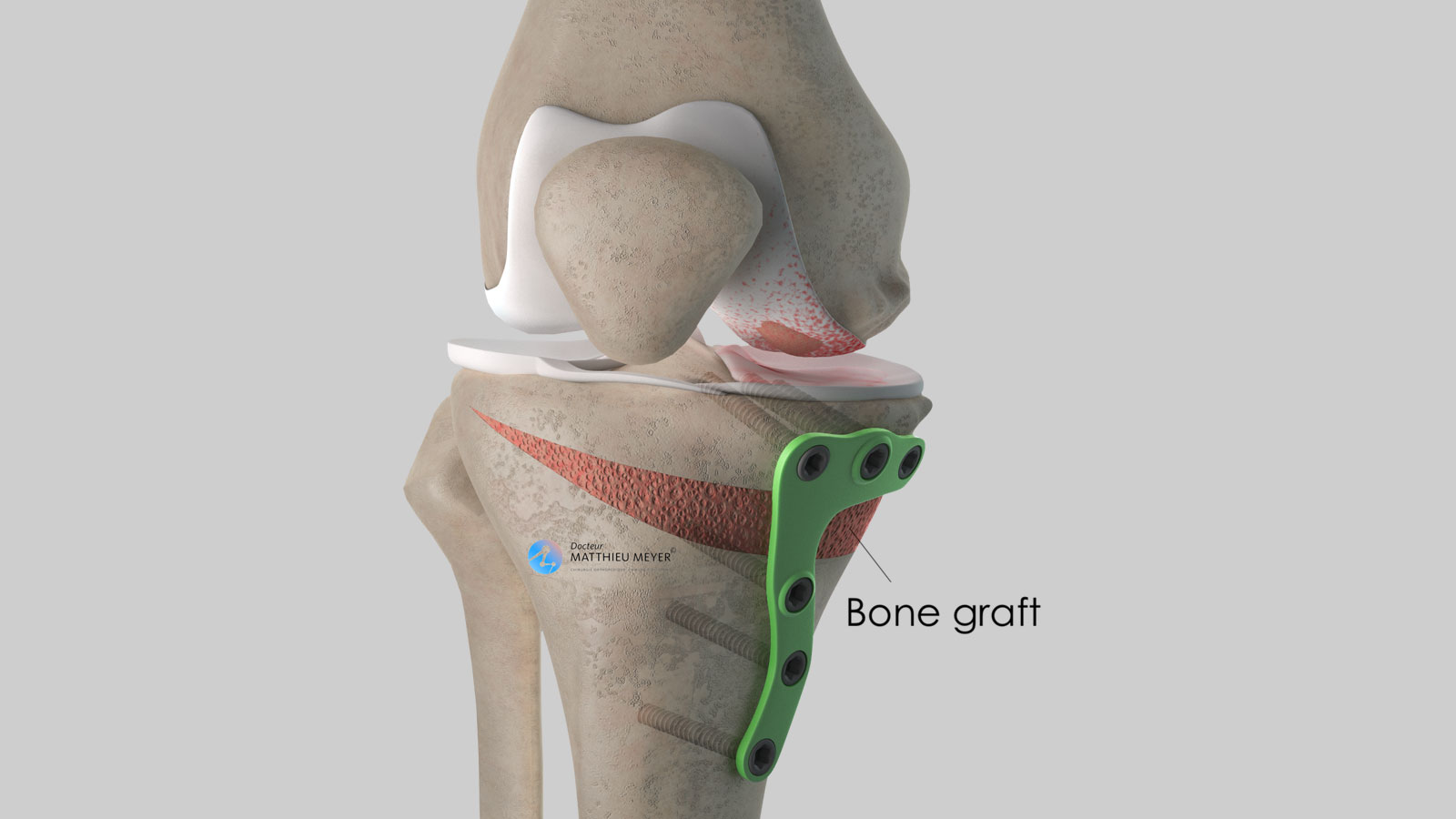
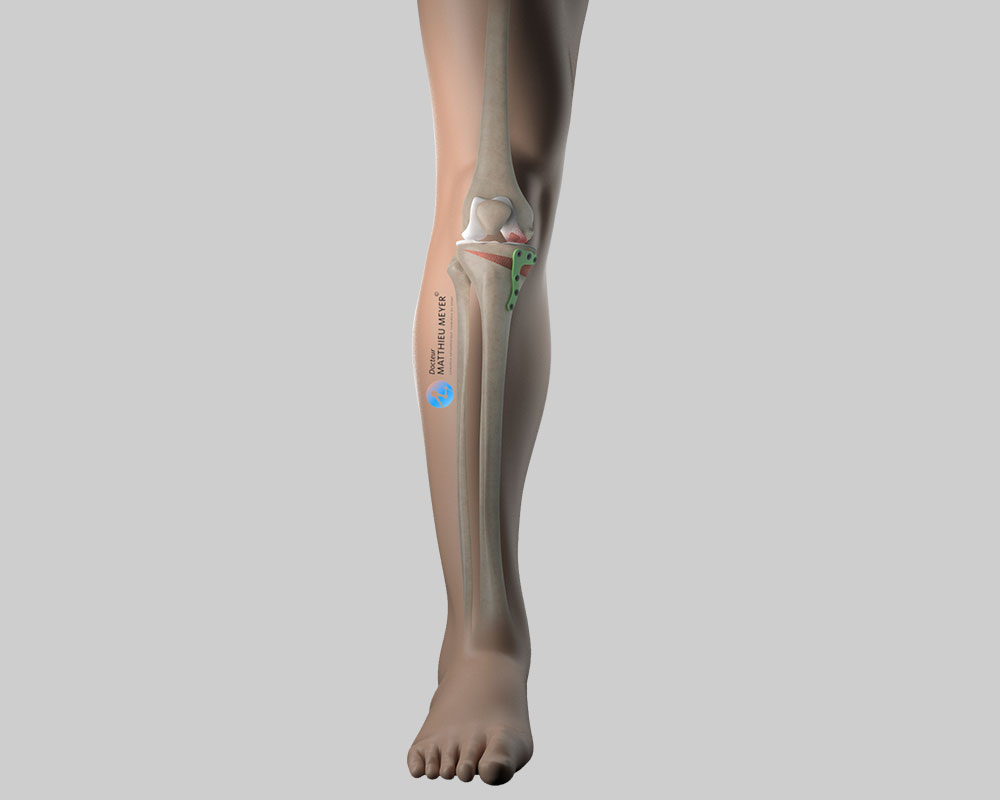
To carry out a high tibial osteotomy, an incision about 10 centimetres long on the higher, medial part of the leg is necessary. A cut is made in the tibia to realign the axis of the leg and a wedge of bone is inserted in the cut to maintain the correction. The bone graft is harvested from the iliac crest of the patient’s pelvis (autograft) or another patient (allograft). In the latter case, the bone is taken from the femoral heads of selected patients who have had a total hip replacement (after questioning and serological tests). This bone is then treated to inactivate any residual microbes or viruses.
Contrary to an organ transplant, a bone allograft does not require antirejection medication.
Once the graft is in place, the tibia is fixed with a plate.
After the operation
A drain is inserted in the wound to prevent the formation of a haematoma.
After the operation, the knee is partially numbed with a nerve block to help improve postoperative pain management.
The effect lasts approximately 18 hours after the operation and can be prolonged with the insertion of a catheter in the thigh if the anaesthetist considers it necessary. Medication and ice on the knee also provide effective postoperative pain management.
After the operation, weight-bearing is not allowed on the leg operated on for 6 weeks and crutches must be used for walking.
Weight-bearing can then be resumed gradually. During this period, the knee can be mobilised during rehabilitation sessions. The knee may be immobilised in a brace while the bone heals.
The stay in hospital is often between 2 and 5 days.
The bone takes 2 to 3 months to heal, sometimes longer.
Several appointments are necessary to monitor the healing of the osteotomy.
The duration of medical leave depends on the patient’s occupation and is often between 2 and 4 months.
Driving can be resumed once weight-bearing is fully recovered. Sport can generally be resumed after 6 months.
Risks linked to the operation
Unfortunately, zero risk does not exist in surgery. Any operation has its risks and limitations, which you must accept or not undergo the operation. However, if an operation is proposed, the surgeon and the anaesthetist consider that the expected benefits far outweigh the risk incurred.
Some risks, such as microbial infections of the surgical site, are common to all types of surgery. Fortunately, this complication is rare but when it occurs requires another operation and a course of antibiotics.
Bruising can also appear around the surgical site. This is usually prevented or reduced with a suction drain inserted at the end of the operation and removed in the days following the operation.
Knee surgery and lack of weight-bearing on the limb operated on also increase the risk of phlebitis, which can lead to a pulmonary embolism. To minimise this risk, blood thinners (in the form of daily injections or tablets) are prescribed until weight-bearing is resumed, in other words, for 6 weeks after the operation.
Failure of the osteotomy to fuse after 6 months is called nonunion and requires further surgery for the tibia to heal.
In rare cases, the knee remains stiff, hot, and painful for several months after the operation. This complication, known as algodystrophy or Chronic Regional Pain Syndrome (CRPS), is unpredictable and sometimes takes a long time to heal.
Finally, rarer complications can also occur. Blood vessels (arteries, veins) can be accidentally damaged and require vascular surgery (bypass). Nerves can also be damaged accidentally during the operation with a risk of paralysis or loss of feeling in the limb operated on, which can be transitory or permanent.
If you have any concerns about the operation, do not hesitate to talk to your surgeon or the anaesthetist and they will answer any questions you may have.
In summary...
When is surgery necessary?
In the case of medial osteoarthritis in young patients (< 60 years)
Aim of the operation
Relieve the pain and slow the progression of osteoarthritis
Which anaesthesia?
General or regional (determined with the anaesthetist)
Duration of hospitalisation
Between 2 and 5 days
Resumption of weight-bearing
6 weeks after the operation
After the operation
Return home
Duration of rehabilitation
Generally 2 to 3 months
Duration of medical leave
2 to 4 months
Resumption of car driving
1 ½ months after the operation, once weight-bearing has been resumed
Resumption of sport
6 months after the operation
Make an appointment
please do not hesitate to contact us or make an appointment online via DoctoLib